Risk factors for first episode of accident encephal vascular brain at different altitude levels
DOI:
https://doi.org/10.37711/rpcs.2020.2.4.224Keywords:
stroke, essential hypertension, altitudeAbstract
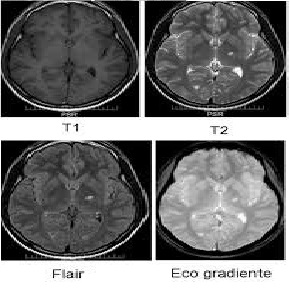
Objective. To determine the risk factors for the first episode of cerebral cerebrovascular accident (CVA) in people living at different levels of altitude. Methods. An observational, cross-sectional and analytical study was carried out in two hospitals located at 150 meters above sea level and 3250 meters above sea level, between 2012 and 2018, the sample was selected according to inclusion and exclusion criteria. The diagnosis of stroke was determined by tomography and / or brain resonance. Results. 72 (100 %) patients were included, 40 (55.5 %) lived at 150 meters above sea level and 32 (44.5 %) at 3250 meters above sea level; the averages of ages were 64.3 + -13.9 and 71.6 + - 14,0 years respectively (p = 0.033). The most affected age group was between 70 and 79 years, the highest percentage in height (43.7 % vs 27.5 %). The most frequent risk factors for stroke at sea level were arterial hypertension (95.0 % vs 62.5 %), diabetes mellitus (47.5 % vs 3.1 %) and atrial fibrillation (15.0 % vs 0.0 %) compared to altitude. The low socioeconomic level (81.2 % vs 27.5 %), the female gender (75.0 % vs 42.5 %), having valve disease (6.2 % vs 2.5 %) and polycythemia (9.3 % vs 0.0 %) were more frequently associated with stroke in height. Conclusions. It is concluded that arterial hypertension is an important risk factor for the first episode of brain stroke both at sea level and at altitude. Diabetes and atrial fibrillation were at sea level and in altitude, the low socioeconomic level, polycythemia, and suffering from valve disease.
Downloads
References
1. Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An Updated definition of stroke for the 21st Century: a statement for health care professionals from the American heart Association/American stroke Association. Stroke.2013;44(7): 2064-89 doi: 10.1161/STR.0b013e318296aeca
2. Roy-O’Reilly M, Mac Cullough L. Sex differences in stroke. The contribution of coagulations. Exp Neurol. 2014; 259: 16-27 [Consultado el 05/01/2018]. doi: 10.1016/j.exp-neurol.2014.02.011
3. Málaga G, De la Cruz-Saldaña T, Busta-Flores P, Carbajal A, Santiago-Mariaca K. La enfermedad cerebrovascular en el Peru: estado actual y perspectivas de investigación clínica. Acta Med Peru. 2018; 35(1): 51-4. [Consultado el 05/01/2018]. Disponible en: http://www.scielo.org.pe/pdf/amp/v35n1/a08v35n1.pdf
4. Davalos LF, Malaga G. El accidente cerebrovascular en el Perú. Una enfermedad prevalente olvidada y desatendi-da. Rev peru med exp salud publica.2014;31(2):400-401 [Consultado el 05/01/2018]. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pi-d=S1726-46342014000200040&lng=es.
5. Bhatnagar A. Environmental determinants of cardiovas-cular disease. Circ Res. 2017 Jul 7; 121(2): 162-180 doi: 10.1161/CIRCRESAHA.117.306458
6. Peñaloza D, Arias-Stella J. The heart and pulmonary circulation at high altitudes: healthy highlanders and chronic mountain sickness. Circulation. 2007; 115(9): 1132-46 [Consultado el 05/01/2014]. disponible en: doi: 10.1161/CIRCULATIONAHA.106.624544.
7. Bigham AW, Wilson MJ, Julian CG, Kiyamu M, Vargas E, León-Velarde, et al. Andean an Tibetan patterns of adaptation to high altitude. Am J Hum Biol. 2013;25(2):190-7 doi: 10.1002/ajhb.2235
8. Epub 2013 Jan 24.8. Ortiz E, Ojeda O, Silva F. Accidente cerebro vascular en poblaciones situadas a grandes alturas: revisión y análisis de los factores de riesgo. Rev Ecuat Neurol.2008; 17(1-3):1-21 [Consultado el 05/01/2015].disponible en: http://revecuatneurol.com/magazine_issue_article/accidente-cerebrovascular-en-poblaciones-situadas-a-grandes-alturas-revision/
9. O Donnell MJ, Siu L, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and Regional effects of potentially modificable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case control study. Lancet 2016;38(10046):761-75 doi: 10.1016/S0140-6736(16)30506-2.
10. Marcotti AC. Estudo dos efeitos da dominancia he-misférica cerebral esquerda sobre o acidente vascular encefálico a través de tres escalas de funcionalidade. Monografias do curso fisioterapia da unioeste. 2009. 1 [Consultado el 05/01/2015]. disponible en: https://www.efdeportes.com/efd142/acidente-vascular-ence-falico-tratamento-cinesioterapeutico.htm
11. Vera-Romero OE, Vera-Romero FM. Evaluación del nivel socioeconómico: presentación de una escala adaptada en una población de Lambayeque. Rev Cuerpo Med. HNAAA.2013;6(1): 41-45 [Consultado el 05/01/2016]. disponible en: https://dialnet.unirioja.es/servlet/articu-lo?codigo=4262712
12. Mancia G, Fagard R, Narkiewicz K, Redón J, Zanche-tti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. The taske force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology. J Hypertension. 2013; 31(7 ):1281-1357 [Consultado el 05/02/2017]. dispo-nible en: https://academic.oup.com/eurheartj/arti-cle/34/28/2159/451304
13. Nishimura RA, Otto C, Bonow R, Carabello B, Erwin J, et al. 2014 AHA/ACC Guideline for the management of pa-tients with valvular Heart Disease: Executive Summary. A Report of The American College of Cardiology / Ame-rican Heart Association Task Force on Practice Guideli-nes. Circulation 2014; 1-96 [Consultado el 05/02/2017]. doi: 10.1161/CIR.0000000000000029
14. Tsai CF, Anderson N, Thomas B, Sudlow CL. Comparing Risk Factor Profiles between Intracerebral Hemorrha-ge and Ischemic Atroke in Chinese and White Popu-lations: Systematic Review and Meta-Analysis. Plos One.2016;11(3):eo151743 [Consultado el 05/02/2017]. https://doi.org/10.1371/journal.pone.0151743
15. Amaru-Lucanu R, Vera-Carrasco O. Guia para el diagnós-tico y tratamiento de las eritrocitosis patológicas en la altura. Rev Med La Paz. 2016;22(2): 70-77 [Consultado el 05/08/2017]. disponible en: http://www.scielo.org.bo/pdf/rmcmlp/v22n2/v22n2_a12.pdf
16. Van Asch CJ, Luitse MJ, Rinkel GJ, Vandertweel I, Algra A, Killon CJ. Incidence, case fatality and functional outcome of intracerebral haemorrhage over time, according to age, sex and ethnic origin: a systematic review and me-taanalysis. Lancet. Neurol.2010; 9(2):167-176 [Consulta-do el 05/08/2017]. doi: 10.1016/S1474-4422(09)70340-0.
17. Liu Y, Xu G, Wu W, Zhang R, Ying Q, Zhu W. Subtypes and one year survival of first-ever stroke in chinese patients: The Nanjing Stroke Registry. Cerebrovasc Dis. 2006,22(2-3):130-136 [Consultado el 05/08/2017]. disponible en: https://doi.org/10.1159/000093241
18. Castañeda-Guarderas A, Beltran-Ale L, Casma-Busta-mante R, Ruiz-Grosso P, Málaga G. Registro de pacientes con accidente cerebrovascular en un hospital público del Perú. 2000-2009. Rev Peru Med Exp Salud Publi-ca.2011.28(4):623-27 [Consultado el 05/08/2017]. disponible en: https://rpmesp.ins.gob.pe/index.php/rp-mesp/article/view/425/425
19. Machado-Alva J, Machado-Duque M. Prevalencia de fac-tores de riesgo cardiovascular en pacientes con dislipi-demia afiliados al sistema de salud en Colombia. Rev Per Med Exp Salud Publica.2013;30(2):205-211 [Consultado el 15/8/2017]. disponible en: http://www.scielo.org.pe/pdf/rins/v30n2/a07v30n2.pdf
20. Prat H. Enfermedad cerebrovascular y estatinas. Rev Chil Cardiol.2012;31(2):148-51 [Consultado el 15/8/2017]. disponible: http://dx.doi.org/10.4067/S0718-85602012000200010.
21. Dhiman D, Mahajan S, Sharma S, Raina R. The evolving pattern and outcome of stroke at moderate. J Neurosci Rural Pract.2018;9(1):68-72 [Consultado el 15/8/2017]. doi: 10.4103/jnrp.jnrp_207_17
22. Castilla-Guerra L, Espino-Montoro A, Fernandez-Moreno MC, Lopez-Chozas JM. Abnormal blood pressure circa-dian rhytm in acute ischaemic stroke; are lacunar strokes really different? Int J Stroke.2009;4(4):257-61 [Consul-tado el 15/8/2017]. https://doi.org/10.1111/j.1747-4949.2009.00314.x
23. Gibson C. Cerebral ischemic stroke: is gender important? J Cereb Blood Flow Metan.2013;33(9):1355-1381 [Consultado el 15/8/2018]. Disponible en: doi: 10.1038/jcbfm.2013.102
24. Castillo JL, Oscanoa TJ. Dislipidemia como factor de riesgo para enfermedad cerebrovascular: estudio casos y controles. Horizonte Medico.2016;16(4): 13-19 [Consultado el 15/9/2018]. disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pi-d=S1727-558X2016000400003
25. Chen R, Ovbiagele B, Feng W. Diabetes and Stroke: Epi-demiology, pathophysiology, Pharmaceuticals and out-comes. Am J Med Sci.2016;351(4):380-386 [Consultado el 15/9/2018]. doi: 10.1016/j.amjms.2016.01.011
26. Cantu-Brito C, Ruiz-Sandoval JL, Murillo-Bonilla LM, Chi-quete E, Leon-Jimenez C, Arauz A, et al. Manejo agudo y pronostico a un año en pacientes mexicanos con un primer infarto cerebral: resultados del estudio multicéntrico PREMIER . Rev Neurol.2010; 51(11):641-49 [Con-sultado el 15/9/2018]. doi: https://doi.org/10.33588/rn.5111.2010527
27. Ariesen MJ, Claus SP, Rinkel GJ, Algra A. Risk factors for intracerebral hemorrhage in the general population: a systemic review. Stroke.2003;34(8):2060-2065 [Consul-tado el 15/9/2018]. disponible en: https://www.aha-journals.org/doi/10.1161/01.str.0000080678.09344.8d
28. Salvetti M, Paini A, Bertacchinini F, Aggiusti C, Stassaldi D, Verzeri L, et al. Therapeutic approach to hypertensive Emergencies: hemorrhagic Stroke. High Blood Press Cardiovascular Prev.2018;25(2):191-195 [Consultado el 5/1/2019]. doi: 10.1007/s40292-018-0262-3.
29. Manning LS, Robinson TG. New Insights into blood Pres-sure control for intracerebral haemorrhage. Front Neu-rol Neuroscie.2015;37:35-50 [Consultado el 15/9/2018]. doi: 10.1159/000437112
30. Sare GM, Geeganage C, Bath PM. High blood pressure in acute ischaemic stroke-broadening therapeutic hori-zons. Cerebrovasc Dise.2009;27 suppl 1:156-61[Consul-tado el 15/9/2017]. doi: 10.1159/000200454.
31. Tsivgoulis G, Katsanos AH, Butcher KS, Boviatsis E, Trian-tafyllou N, et al. Intensive blood pressure reduction in acute intracerebral hemorrhage: a meta-analysis. Neuro-logy. 2014;21:83(17):1523-9 [Consultado el 15/9/2017]. disponible en: doi: 10.1212/WNL.0000000000000917
32. Chen Z, Iona A, Parish S, Chen Y, Guo Y, Bragg F, et al. Adi-posity and risk of ischaemic and haemorrhagic stroke in 0.5 million Chinese men and women: a prospective cohort study. Lancet Glob Health.2018;6(6):e630-e640 [Consultado el 15/1/2019]. doi: 10.1016/S2214-109X(18)30216-X
33. Bazzano L, Gu D, Whelton M, Wu X, Chen CS, Duan X, et al. Body mass index and risk of stroke among chinese men and womwn. Ann Neurol.2010;67(1):11-20 [Consul-tado el 15/9/2017]. doi: 10.1002/ana.21950
34. Kroll ME, Green J, Beral V, Sudlow CL, Brown A, Kirichek D, et al. Adiposity and ischemic and hemorrhagic stroke: prospective study in women and meta-analysis. Neuro-logy.2016;87(14):1473-1481 [Consultado el 15/1/2019]. doi: 10.1212/WNL.0000000000003171.
35. Gloekler S, Saw J, Koskinas KC, Kleinecke C, Jung W, Nietlispach F, et al. Left atrial appendage closure for pre-vention of death stroke and bleeding in patients with nonvalvular atrial fibrillation. Int J Card.2017;15:234-246 [Consultado el 15/5/2019]. disponible en: doi: 10.1016/j.ijcard.2017.08.049
36. Safavi-Naeini P, Rasekh A. Closure of left atrail appenda-ge to prevent stroke: Devices and status. Tex Heart Inst J. 2018;45(3):172-174 [Consultado el 15/2/2019]. disponi-ble en: doi: 10.14503/THIJ-18-6693
37. Skurk C, Leistner DM, Park JW, Landmesser V. Catheter-ba-sed closure of the left atrial appendage: Stroke prevention in atrial fibrillation. Internist. 2016;57(9):844-55 [Consulta-do el 15/2/2018]. doi: 10.1007/s00108-016-0113-z.
38. Chanda A, Reilly JP. Lef atrial appendage occlusion for stroke prevention. Progr Cardiovasc.2017;59(6):626-635 [Consul-tado el 15/2/2018]. doi: 10.1016/j.pcad.2017.04.003.
39. Ruiz L, Peñaloza D. Altitude and hypertension. May Clin Proc.1977,52(7):442-5 [Consultado el 15/2/2017]. dispo-nible en: https://pubmed.ncbi.nlm.nih.gov/875468/
40. Marmot MG, Shipley MJ, Rose G. Inequalities in dea-th--specific explanations of a general pattern? Lancet. 1984;1:1003–6 [Consultado el 15/2/2017]. disponible en: https://www.sciencedirect.com/science/article/abs/pii/S0140673684923377
Downloads
Published
Issue
Section
License
Copyright (c) 2020 Jose Antonio Romero Cordova, Aníbal Valentín Díaz Lazo

This work is licensed under a Creative Commons Attribution 4.0 International License.