Febrile neutropenia in oncohematological patients: a bibliographic review on bacteriological profle and resistance in Latin America
DOI:
https://doi.org/10.37711/rpcs.2022.4.4.391Keywords:
Febrile neutropenia, Microbial susceptibility tests, Microbial Drug Resistance, Bacterial infectionsAbstract
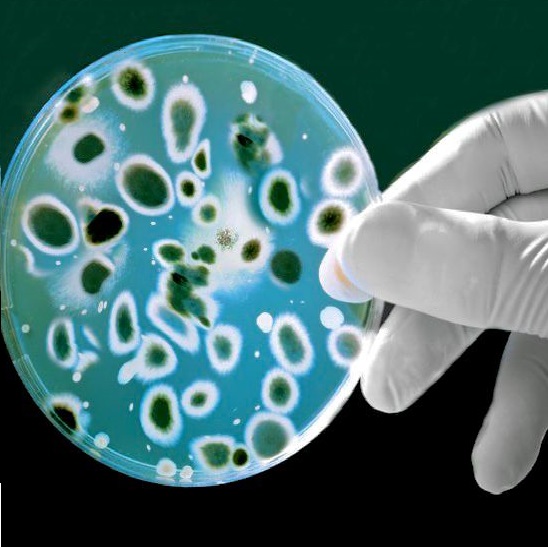
Objective. To describe febrile neutropenia in oncohematological patients in Latin America, its bacteriological profle and resistance. Methods. A systematic review study was carried out, following PRISMA criteria in order to respond to the research objective. Information was collected from observational studies, review articles, meta-analysis, systematic reviews, in English and Spanish. The review was carried out in the LILACS, PubMed, ScienceDirect and SciELO databases, using Medical Subject Headings (MeSH) terms and health sciences descriptors (DeCS) for the search strategy. Results. A total of 9 articles were selected, showing that the predominant germs associated with patients with febrile neutropenia are gram-negative bacilli, with Escherichia coli being the main and least resistant. On the other hand, Klebsiella pneumoniae and Pseudomona aeruginosa are more resistant gram-negative microorganisms, causing more severe infection. The antimicrobials with good efcacy and absence of resistance against these pathogens are carbapenemics, amikacin, meropenem and tigecycline. Staphylococcus aureus and Staphylococcus epidermidis are the main grampositive agents found, with a wide resistance and 100% sensitivity to linezolid, daptomycin and vancomycin. Conclusions. Colombia is the country with the highest antimicrobial resistance in Latin America. However, there is an increase in resistant bacteria over time, due to incorrect use of antimicrobials, omission of microbiological examinations and lack of scientifc evidence; therefore, it is important to carry out quantitative microbiological studies in Latin American countries in order to establish empirical treatment with good results.
Downloads
References
Rivas J. Neutropenia febril: el punto de vista del hematólogo. Gaceta Mexicana de oncología. 2016 Jul 1; 15(4): 212-21.
Agrawal A, Feusner J. Chapter 33 - Supportive Care of Patients with Cancer. En: Lanzkowsky P, Lipton J, Fish J, editores. Lanzkowsky’s Manual of Pediatric Hematology and Oncology. 6a ed. [Internet]. San Diego: Academic Press; 2016 [Consultado 2022 Jul 10]. 620-55. Disponible
en: https://www.sciencedirect.com/science/article/pii/B9780128013687000338
Calderón J, Cercado A. Etiología bacteriana y susceptibilidad antibiótica en adultos con leucemias agudas y neutropenia febril con factores de alto riesgo. Oncología (Ecuador). 2021 Abr 30; 31(1): 74-85.
Gustinetti G, Mikulska M. Bloodstream infections in neutropenic cancer patients: A practical update. Virulence. 2016 Mar 22; 7(3): 280-97.
Hakim H, Flynn P, Knapp K, Srivastava D, Gaur A. Etiology and clinical course of febrile neutropenia in children with cancer. Pediatr Hematol Oncol. 2009 Sep; 31(9): 623-9.
Cuervo S, Bermúdez C, Enciso L, Gómez J, Castillo J, Sánchez R, et al. Guía de práctica clínica para el diagnóstico y el tratamiento de las infecciones bacterianas y micóticas en pacientes oncológicos mayores de 15 años con neutropenia febril posquimioterapia de alto riesgo. Revista Colombiana de Cancerología. 2014 Oct 1; 18(4): 186-96.
Soliz C, Caamaño C, Coloma E, Rodríguez A, Ramírez N. Prevalencia de gérmenes con multirresistencia antibiótica en bacteriemia asociada a neutropenia febril en pacientes oncológicos hospitalizados: Un estudio de centro único. Oncología (Ecuador). 2022 Ago 6; 32(2): 157-68.
Alberto F. Resistencia antibiótica en bacilos gram negativos, cocáceas gram positivas y anaerobios. implicancias terapéuticas. Rev Med Clin Condes. 2014 May 1; 25(3): 432-44.
Taplitz R, Kennedy E, Bow E, Crews J, Gleason C, Hawley D, et al. Outpatient Management of Fever and Neutropenia in Adults Treated for Malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America Clinical Practice Guideline Update. JCO. 2018 May 10; 36(14): 1443-53.
Joncour A, Puyade M, Michaud A, Tourani J, Cazenave F, Rammaert B. Is current initial empirical antibiotherapy appropriate to treat bloodstream infections in short-duration chemo-induced febrile neutropenia? Support Care Cancer. 2020 Jul; 28(7): 3103-11.
Ramos A, Pintos I, Múñez E. Protocolo diagnóstico y tratamiento de la neutropenia febril. Medicine - Programa de Formación Médica Continuada Acreditado. 2018 May
; 12(55): 3272-6.
Zimmer A, Freifeld A. Optimal Management of Neutropenic Fever in Patients with Cancer. J Oncol Pract. 2019 Ene; 15(1): 19-24.
Naurois J, Novitzky I, Gill M, Marti F, Cullen M, Roila F, et al. Management of febrile neutropenia: ESMO Clinical Practice Guidelines. Ann Oncol. 2010 May; 21(5): 252-6.
Maldonado M, Acuña M, Álvarez A, Avilés C, de la Maza V, Salgado C, et al. Microorganisms isolated from blood cultures in children with cancer and high-risk febrile neutropenia from fve hospitals in Santiago, Chile, 2012-2015. Revista chilena de infectología. 2018 Abr; 35(2): 140-6.
Bello A, Cuesta M, Díaz M, Mendoza L, Sarmiento P. [Microbiological characterization and antimicrobial susceptibility pattern of infections associated with febrile neutropenia in pediatric hemato-oncological patients.]. Andes Pediatr. 2022 Feb; 93(1): 65-77.
Garzón J, Isaza N, Posada A, Mendez R, Arenas J, Ardila M, et al. Características clínicas y microbiológicas de pacientes con neutropenia febril en un hospital Universitario. Infectio. 2019; 347-51.
Barroso G, Quintero Y, Rivas Y. Diagnóstico y tratamiento de la neutropenia febril en el paciente oncohematológico. Revista Cubana de Hematología, Inmunología y Hemoterapia [Internet]. 2020 Dic [Consultado 2022 Nov 2]; 36(4). Disponible en: http://scielo.sld.cu/scielo.php?script=sci_abstract&pid=S0864-02892020000400002&lng=es&nrm=iso&tlng=es
Moreno F, Gomez B. Antibiotic Management of Patients with Hematologic Malignancies: From Prophylaxis to Unusual Infections. Curr Oncol Rep. 2022 Jul; 24(7): 835-42.
Guerrini G, Peretti H, Calgmaggi A. Complicaciones infecciosas en pacientes con leucemia mieloide aguda. Actualizaciones en Sida e Infectología [Internet]. 2018 Jul 1 [Consultado 2022 Oct 30]; Disponible en: https://revista.infectologia.info/index.php/revista/article/view/26
Cortés D, Maldonado M, Rivacoba M, de la Maza V, Valenzuela R, Payá E, et al. Caracterización clínica y microbiológica de episodios de bacteriemia por Streptococcus
grupo viridans en niños con cáncer y neutropenia febril de alto riesgo. Rev chil infectol. 2020; 383-8.
Loiudice N, Verdinelli C. Neutropenia febril. Análisis de casos en un centro de tercer nivel de atención. Rev Asoc Med Bahía Blanca. 2020; 9-19.
Peña T, Rojas J, Benavidez R, Gómez T, Cadavid D, Ávila D, et al. Características de los pacientes adultos con neutropenia febril en un hospital universitario (Medellín, 2012-2016). Medicina UPB. 2019 Dic 15; 38(2): 108-13.
García K, Londoño J, Villegas L, González M, Correa A. Microbiological diagnosis in febrile neutropenia secondary to chemotherapy for hematologicmalignancy. A cohort description. Acta méd colomb. 2020; 25-31.
Herrera C, Córdova E, Badía M, Gomez N, Cornistein W, Oviedo V, et al. La era de los microorganismos multirresistentes: impacto en pacientes neutropénicos febriles.
Actual SIDA infectol. 2019; 31-8.
Cataño D, Marín D, Rivera J, Martínez J, Sánchez J, Martínez M, et al. Neutropenia febril asociada a quimioterapia en pacientes con neoplasias hematológicas de un centro
de referencia en Colombia: características clínicas y desenlaces. Revista Salud Uninorte. 2019 Ago; 35(2): 205-20.
Levene I, Castagnola E, Haeusler G. Antibiotic-resistant Gram-negative Blood Stream Infections in Children With Cancer: A Review of Epidemiology, Risk Factors, and Outcome. Pediatr Infect Dis J. 2018 May; 37(5): 495-8.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Andrés Felipe Mercado González, David Abril, Adrián Reibán, Tatiana Palacios

This work is licensed under a Creative Commons Attribution 4.0 International License.